65 year old female with difficulty in walking
Jaya, 9 sem
Roll no 47
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
Date of admission : 29/03/2022
CASE :
A 65 year old female, herder by occupation, bought to the opd with chief complaints of
~Generalised weakness since 1year
~Pain of right fingertips since 2 months
~Dryness of mouth and inability to swallow since 2 months
~H/o fall on 28/3/22 at 8 PM and 29/3/22 at 3 AM
HOPI :
• Patient was apparently asymptomatic 4 years back. Later after the death of her husband , her family members took her to the hospital because she was experiencing weakness. Then she was tested and diagnosed with diabetes mellitus and she is on regular oral medication since then.
She developed ringing sensation and pain in ears on and off since 2 years. She also complains of fullness in the ear. Not associated with any discharge or loss of hearing.aggrevated by journey . She says that it decreases on taking medication.( Dolo or they will take her to local rmp). But the ringing sensation does come up occasionally.
• Dryness of mouth since 2 months associated with difficulty in swallowing. It was insidious in onset and gradually progressive. The difficulty in swallowing is more for solids than liquids. She apparently can only swallow if she drinks water along with her food. It is associated with loss of appetite and early satiety. She feels like her voice has also changed as she feels pain on trying to talk.
• Pricking type of Pain of right fingertips since 2 months, which is constant, increases on activity such as mixing food or combing hair so she stopped doing house chores and sleeps most of the time.
There is discoloration at the tips of fingers.
•2 months back, after getting down the bus, she landed on a sloped surface, lost her balance and tumbled down. She lost her consciousness for 5 minutes and was later woken up by her daughter and was given water. She walked back home after this episode. She had trauma to head and laceration on her left arm.
They came to the hospital on 16/3/23 they advised medicine for which they informed due to some reason they went home
• again She has history of fall on 28/3/22 at 8pm when she went to take a bath, she sat on a stool and fell back.
•At 3 AM, she woke up to urinate, went to the washroom and sat in squatting position, before she could support herself with her hands she fell on her face and that resulted in a swollen right eye.
PAST HISTORY :
She has deviation of mouth since age of 5months on right side
She is a known case of diabetes mellitus since 4 years and she is on regular medication.
PERSONAL HISTORY :
Diet : Mixed
Appetite : Decreased
Bowel and bladder movements : Regular
Sleep : Disturbed
No allergies
No addictions
MENSTRUAL HISTORY :
Attained menopause
GENERAL EXAMINATION :
Patient is conscious, coherent , co-operative and oriented to time, place and person.
Well built and well nourished.
Pallor is present.
No icterus, cyanosis, clubbing, generalized lymphadenopathy and bilateral pedal edema.
VITALS:
PR: 90bpm
BP: 110/70mmHg
RR: 16cpm
Temperature: Afebrile
SYSTEMIC EXAMINATION :
CVS: S1 S2 present
No murmurs, thrills heard.
RS: BAE present, NVBS heard.
CNS: E4V5M6
HMF: intact. Conscious.
Tone: R. L
UL. N. N
LL. N. N
Power: R. L
UL. 5/5. 5/5
LL. 5/5. 5/5
Rhomberg sign - negative
Investigations:
30/3/22
HB 8.3
PCV 24.1
MCV 89.6
PLT 1.87 L
RBS: 164 mg/dl
29/3/22 30/3/22
Se. Creatinine: 2.4mg/ dL
Se. Uric acid: 11.1 mg/dL 11.5mg/dL
Blood urea: 41 mg/dL
Na: 138 mEq/L
K: 4.8 mEq/L
Cl: 101 mEq/L
LFT:
Db: 0.16 mg/dL
Tb: 0.57 mg/dL 0.60 mg / dL
AST: 64 IU/L 55IU/ L
ALT: 57 IU/L 52 IU/L
ALP: 204 IU/L
TP: 8.0 gm/dL
Albumin: 3.6 gm/dL 3.53
A/G ratio: 0.89
Chest X-ray
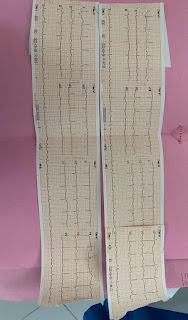
Ecg :
ENT REFERAL :
Direct laryngoscopy
( done in other hospital before admission)
Doppler 2d echo:
Ophtha referal :
X- rays :
Provisional Diagnosis:
Crest syndrome?
RAYNAUDS phenomenon with scleroderma ??
Treatment plan:
29 /3/22
1. Tab. NIFEDIPINE 10mg TID
2. IV FLUIDS 2 NS
3. Inj. ACTRAPID 10 units
(Morning- afternoon-night)
4. Tab. FOLITRAX ( methotrexate)7.5mg once a week
Every Wednesday
5. Tab.FOLIC ACID 5mg once a week on Tuesday.
Pantoprazole
30/3/22
1. Tab. NIFEDIPINE 10mg TID
2. IV FLUIDS 2 NS
3. Inj. ACTRAPID 10 units
(Morning- afternoon-night)
4. Tab. FOLITRAX ( methotrexate)7.5mg once a week
Every Wednesday
5. Tab.FOLIC ACID 5mg once a week on Tuesday.
6.GRBS 6th hourly (8.am,2.pm,8pm, 2am)
31/3/22
1. Tab. NIFEDIPINE 10mg TID
2. IV FLUIDS 2 NS
3. Inj. ACTRAPID 10 units
(Morning- afternoon-night)
4. Tab. FOLITRAX ( methotrexate)7.5mg once a week
Every Wednesday
5. Tab.FOLIC ACID 5mg once a week on Tuesday.
6.GRBS 6th hourly (8.am,2.pm,8pm, 2am)
7.T.LYSER-D (2 BD)
8.T.PAN 40 mg OD
9.T. LIMCEe 500mg afternoon
1/4/22
1. Tab. NIFEDIPINE 10mg TID
2. IV FLUIDS 2 NS
3. Inj. ACTRAPID 10 units
(Morning- afternoon-night)
4. Tab. FOLITRAX ( methotrexate)7.5mg once a week
Every Wednesday
5. Tab.FOLIC ACID 5mg once a week on Tuesday.
6.GRBS 6th hourly (8.am,2.pm,8pm, 2am)
7.T.LYSER-D (2 BD)
8.T.PAN 40 mg OD
9.T. LIMCEe 500mg afternoon

























Comments
Post a Comment